
Background: Langerhans cell histiocytosis (LCH) is the most common histiocytic disorder that is now recognized as a neoplasm by the World Health Organization. It is generally classified based on the site and extent of disease involvement (single system or multisystem). Pulmonary LCH (pLCH), an uncommon interstitial lung disease associated with smoking, often presents as isolated pulmonary disease. It is unclear whether patients with clinically isolated pLCH have extra-pulmonary lesions at diagnosis or during the course of their disease. The role of [18F] fluorodeoxyglucose positron emission tomography-computed tomography (FDG-PET-CT) in the staging of pLCH remains unclear. Our study aims to better characterize the utility of radiographic staging studies at time of diagnosis and prevalence of extrapulmonary disease at follow up in pLCH.
Methods: We conducted a retrospective study of patients presenting with clinical findings consistent with isolated pLCH seen at the Mayo Clinic from January 2000 to January 2020. All patients had a diagnosis of pLCH determined by chest imaging studies [computed tomography (CT) or high-resolution CT (HRCT)] or by histopathologic findings from surgical or transbronchial lung biopsy. Histopathologic findings for the diagnosis of pLCH required the presence of Langerhans cells (S100+/CD1a+/Langerin+). Patients were excluded if they had clinically apparent extra-pulmonary organ involvement at the time of diagnosis. BRAF V600E mutation was determined by immunohistochemistry (IHC) or cell-free DNA (cfDNA). Staging was defined as FDG-PET-CT or whole body CT imaging obtained within 3 months of diagnosis of pLCH. Extra-pulmonary LCH involvement was determined by imaging characteristics or by histopathologic findings. Descriptive statistics and overall survival (OS) were analyzed with JMP software, version 14 (SAS Institute Inc., Cary, NC).
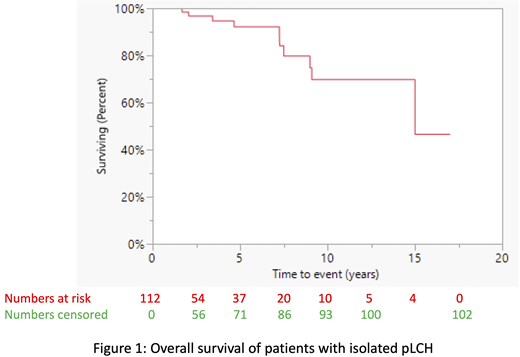
Results: A total of 112 patients with clinically isolated pLCH were identified. The median age at diagnosis was 45 years (range 21-73), and 48 (43%) were male. The majority (n=110, 99%) were former or current smokers with a median pack year of 25 (range 1-57). Three (3%) patients were noted to have occupational industrial exposure. Nine patients had a history of another cancer prior to their diagnosis and staging of pLCH [lung (n=4), breast (n=2), neuroendocrine (n=2), thyroid (n=1)]. Presenting symptoms included dyspnea on exertion 49 (44%), cough 18 (16%), chest pain 14 (13%), and 29 (28%) were incidentally discovered on imaging studies. On HRCT, the following characteristics were observed: 42 (38%) cystic, 32 (29%) cystic and nodular, 37 (33%) nodular, 1 (<1%) ground glass opacities. Seventy (63%) patients had lung biopsy confirmation, of which 11 (16%) patients underwent BRAF V600Emutation testing (7 by IHC, 4 by cfDNA). Six (55%) of these 11 patients were positive for BRAF V600E mutation. 34 (30%) patients underwent radiographic staging studies within 3 months of diagnosis of pLCH (25 FDG-PET-CT and 9 whole-body CT), and none of these imaging studies showed evidence of extra-pulmonary disease. Of the patients who had at least one year of follow-up (n=52), one (2%) developed extra-pulmonary disease. This patient did not undergo initial staging studies, developed headaches and was found to have a large calvarial lytic lesion within 2 months of pLCH diagnosis (BRAF V600E+). Among those who did not undergo staging at diagnosis (n=78), long term (>5 years) follow up data were available for 23 (29%), and none developed extra-pulmonary disease as determined by clinical notes or imaging studies. No patient had evidence of new extra-pulmonary involvement or second malignancy at the time of last known follow-up. After a median follow-up duration of 2.4 years (95% CI: 1.5-3.6, range: 0.1-17) ten (9%) patients died, of which 5 died of pLCH related complications. The median OS for entire cohort was 15 years (95% CI 9.1-not reached, Figure 1).
Conclusion: Our study shows that adult patients with clinically isolated pLCH rarely present with extra-pulmonary manifestations at diagnosis or at follow up. These findings suggest a limited role of routine radiographic staging studies in pLCH unless clinically indicated. Studies on longer follow up of this cohort would provide further insights into the natural history of pLCH and are underway.
Bennani:Purdue Pharma: Other: Advisory Board; Verastem: Other: Advisory Board; Kite/Gilead: Research Funding; Affimed: Research Funding. Shah:Dren Bio: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal